
Stephen Rush, MD
Professor Associado de Psiquiatria Clínica e Neurociência Comportamental
Psicose Secundária
As experiências psicóticas são comuns nas pessoas a quem é diagnosticada esquizofrenia. De facto, a presença de sintomas psicóticos pode levar ao diagnóstico desta perturbação cerebral se tanto os delírios como as alucinações estiverem presentes durante seis meses, incluindo um mês de sintomas persistentes. Noutras especialidades médicas, o diagnóstico é frequentemente feito após um exame físico, exames de imagem (raios X ou TAC) e análises ao sangue, que são cruciais para determinar o diagnóstico e o tratamento adequado. No entanto, em psiquiatria, este mesmo processo de diagnóstico não produz frequentemente muita informação útil, exceto no caso de psicose secundária (causada por outras perturbações médicas).
A psicose secundária é um termo utilizado com mais frequência nas últimas décadas, uma vez que existe uma perceção crescente de que é vital compreender quando é que sintomas como delírios e alucinações se devem a uma doença ou substância médica conhecida. Anteriormente referido como "funcional" quando tinha uma origem psicológica e "orgânico" quando havia uma origem biológica identificável, a mudança para "primário" e "secundário" reflecte a compreensão de que todas as doenças e sintomas psiquiátricos têm um componente biológico. Este entendimento apareceu pela primeira vez na versão revista da quarta edição do Manual de Diagnóstico e Estatística das Perturbações Mentais (DSM-IV-TR) em 2000. Qualquer substância, medicamento prescrito ou condição médica que afecte o sistema nervoso central pode resultar em sintomas psiquiátricos, incluindo psicose, e, infelizmente, continuamos a assistir a casos em que é feito um diagnóstico presuntivo de esquizofrenia antes de uma avaliação médica completa confirmar a ausência de uma fonte de psicose secundária.
Num artigo de 2016 publicado no The Primary Care Companion to CNS Disorders, o Dr. João Gama Marques estudou a frequência com que os doentes inicialmente diagnosticados com esquizofrenia tinham uma fonte subjacente de psicose secundária que não foi reconhecida. Esta análise retrospetiva de 250 doentes em Portugal demonstrou que 25% dos doentes diagnosticados com esquizofrenia tinham, de facto, uma condição médica subjacente que causava sintomas psicóticos. Além disso, o atraso médio no diagnóstico correto foi de 12 anos. As consequências deste atraso no diagnóstico podem ter consequências devastadoras para os doentes e para os seus familiares.
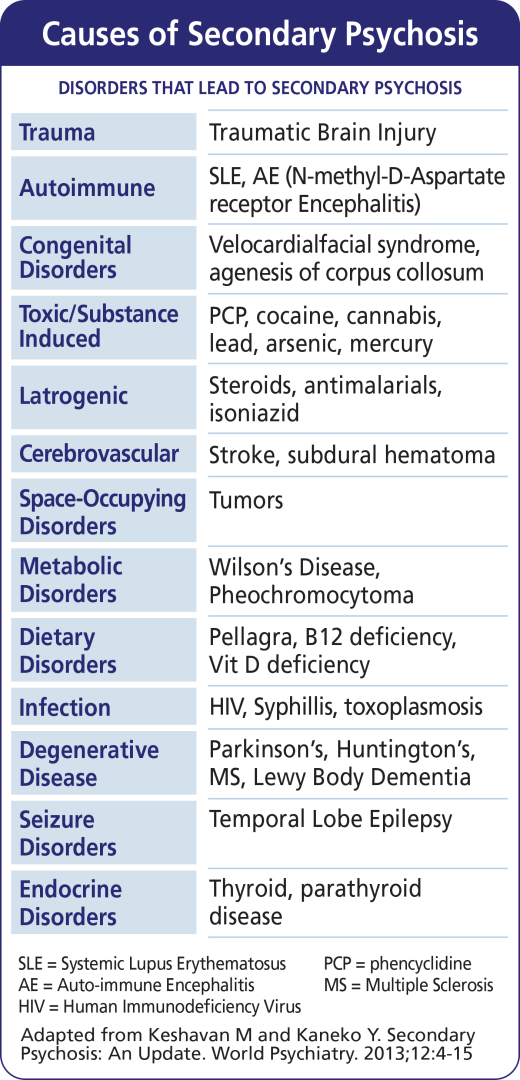
Através da pesquisa de cientistas feita ao longo de décadas e séculos, podemos agora dizer que a psicose secundária pode resultar de 13 grupos principais de distúrbios identificados no gráfico a seguir.
Como é que os médicos determinam se uma perturbação psicótica é "primária" ou "secundária"? Em primeiro lugar, deve ser identificada a substância causadora ou a condição médica. De seguida, deve ser identificada a relação entre a condição médica ou a substância utilizada e os sintomas psicóticos. Ao fazê-lo, os médicos devem considerar três aspectos fundamentais dos sintomas do doente: atipicidade, temporalidade e explicabilidade.
Deve-se suspeitar de uma causa médica subjacente de psicose se a apresentação for atípico no que diz respeito à idade de início e ao tipo de sintomas observados. Por exemplo, a presença de vários tipos de alucinações (auditivas, visuais, tácteis e olfactivas) não é típica da esquizofrenia e aumenta a probabilidade de uma perturbação psicótica secundária, como as observadas na demência ou em alguns tipos de epilepsia. A temporalidade dos sintomas, ou quando eles ocorrem, devem ser considerados quando os sintomas psicóticos seguem o início de uma doença médica ou ingestão de uma substância e desaparecem quando a condição médica melhora ou a substância é eliminada do corpo. Finalmente, como as comorbidades médicas são muito comuns em pessoas com esquizofrenia, é importante perguntar se os sintomas presentes são os melhores explicou por uma perturbação psicótica primária ou secundária. Por exemplo, num doente com uma forte história familiar de esquizofrenia nos seus pais e irmãos, os sintomas psicóticos de longa duração, mesmo no contexto de uma doença médica concomitante, podem ser explicados com maior precisão pela esquizofrenia, dada a predisposição genética presente.
Em abril de 2018, o Centro Médico da Universidade de Cincinnati instituiu o programa First Episode Evaluation and Services (FEELs). Este programa inclui uma equipa multidisciplinar de médicos, enfermeiros, assistentes sociais, farmacêuticos, psicólogos, terapeutas ocupacionais e recreativos que trabalham em conjunto para excluir causas secundárias de psicose em doentes nos primeiros 2 anos após o início dos sintomas, enquanto se encontram numa unidade de internamento de psiquiatria. Este trabalho inclui análises sanguíneas completas, imagiologia, revisão de quaisquer medicamentos tomados e substâncias e testes psicológicos. Esta avaliação ajuda a equipa de tratamento a identificar a causa mais provável da psicose num determinado doente e a orientar o tratamento. Se for identificada uma condição médica, os médicos especializados no tratamento dessa condição envolvem-se no tratamento. Este protocolo foi inspirado no trabalho com doentes cujas perturbações psicóticas secundárias não foram identificadas numa fase inicial da doença, o que teve consequências negativas a longo prazo. Embora muitos centros médicos académicos tenham procedimentos semelhantes, existe ainda uma falta de sensibilização para as causas identificáveis da psicose secundária em muitos locais do mundo. Tanto os médicos como os doentes e os familiares devem ser informados sobre estas questões e defender a avaliação normalizada das causas secundárias de psicose para promover o nosso objetivo comum de cura através de um diagnóstico e tratamento corretos.
Referências:
Keshavan MS, Kaneko Y. Psicoses secundárias: uma atualização. Psiquiatria Mundial. 2013;12(1):4-15. doi:10.1002/wps.20001
Gama Marques J. Psicose orgânica causando esquizofrenia secundária em um quarto de uma coorte de 200 pacientes previamente diagnosticados com esquizofrenia primária. prima
Distúrbio do SNC do Care Companion. 2020;22(2):19m02549.

